A new AI pipeline now spots extranodal extension (ENE) on CT scans of HPV‑positive oropharyngeal cancer with impressive accuracy, giving clinicians a reliable, automated read that links directly to survival outcomes. The system reaches an AUC of 0.81 and outperforms expert neuroradiologists, helping you make more informed treatment choices in everyday practice.
Why Extranodal Extension Matters
In head‑and‑neck oncology, ENE has long guided staging and treatment intensity. Although the latest AJCC guidelines downplay ENE for HPV‑positive tumors, recent evidence shows that imaging‑detected ENE still predicts a higher risk of recurrence and distant disease. Radiologists often rely on subjective visual cues, leading to low inter‑reader agreement and uncertainty in patient management.
How the AI Model Works
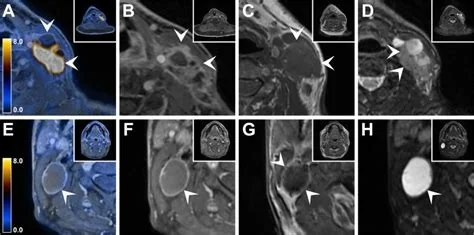
Researchers trained an end‑to‑end deep‑learning workflow on pretreatment planning CTs collected over a decade. The process unfolds in two steps:
- Segmentation: An nnU‑Net architecture automatically outlines lymph‑node gross tumor volumes.
- Classification: A hybrid classifier blends radiomic and deep‑learning features to decide whether each node exhibits ENE.
When benchmarked against neuroradiologists, the AI not only matched human accuracy but also showed a stronger statistical link to overall survival, recurrence‑free survival, and distant disease control. In multivariable analysis, AI‑predicted ENE remained an independent prognostic factor with a hazard ratio exceeding 12 for distant control.
Clinical Impact and Treatment Decisions
The AI read can sharpen treatment de‑escalation strategies. If the model flags ENE, you might consider intensified systemic therapy or tighter imaging surveillance, rather than assuming a uniformly favorable prognosis based solely on HPV status. Conversely, patients without AI‑detected ENE could safely avoid overtreatment, reducing unnecessary toxicity.
Key Benefits
- Objective assessment that reduces variability between readers.
- Direct prognostic relevance tied to survival outcomes.
- Potential to level the playing field for centers lacking dedicated head‑and‑neck neuroradiology expertise.
Implementation Challenges
Adoption won’t happen overnight. Prospective validation, seamless integration with existing PACS workflows, and regulatory clearance are essential steps. Institutions will need to train staff, ensure data privacy, and establish quality‑control protocols before the AI can become a routine part of the diagnostic arsenal.
Patient Scenario
Imagine a 58‑year‑old non‑smoker diagnosed with HPV‑positive cancer. His CT shows several enlarged nodes, but the radiology report is equivocal on ENE. The AI runs in the background, flags one node as ENE‑positive, and the tumor board decides on a modest boost of systemic therapy. Six months later, his scans are clear, and he avoids the higher‑dose radiation that might have been used without the AI insight.
Looking Ahead
As more institutions plug similar models into their imaging suites, the line between “high‑risk” and “low‑risk” HPV‑positive cancer will become far less blurry. The technology promises a practical step toward more precise, data‑driven care, turning a once‑subjective imaging feature into a reliable biomarker you can trust at the bedside.