A machine‑learning model developed by researchers at Nagoya University dramatically improves one‑year survival predictions for patients with spinal metastasis, using five easily obtained pre‑operative factors. The AI‑based scoring system helps clinicians decide between surgical stabilization and palliative care by providing accurate risk stratification, ultimately supporting personalized treatment planning and improving quality of life.
New AI‑Driven Prognostic Model
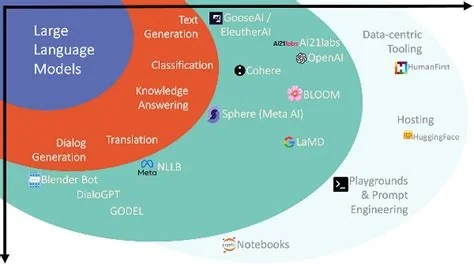
The model was built from a multicenter cohort of 401 patients who underwent spinal surgery across Japan. Using Least Absolute Shrinkage and Selection Operator (LASSO) logistic regression, the algorithm automatically identified the most predictive variables for one‑year overall survival.
Key Pre‑operative Variables
- Vitality index – reflects patient motivation and psychological health.
- Age – distinguishes patients aged 75 years or older.
- ECOG performance status – standard measure of functional impairment.
- Bone metastases outside the spine – presence indicates broader disease spread.
- Pre‑operative opioid use – high doses are linked to immunosuppression.
Model Performance
The scoring system achieved an area under the receiver operating characteristic curve (AUROC) of 0.762, demonstrating strong discriminative ability. Calibration analysis showed close agreement between predicted and observed survival rates. When patients were grouped into low, intermediate, and high risk, one‑year survival probabilities were 82.2 %, 67.2 %, and 34.2 % respectively.
Clinical Impact
Spinal metastasis often causes severe pain, neurological deficits, and reduced mobility. Surgical stabilization can extend ambulation and relieve pain, but it is justified only when expected survival supports the intervention. Traditional scoring systems were derived from data collected before modern targeted therapies and immunotherapies, limiting their relevance today.
Decision‑Making for Surgery vs. Palliative Care
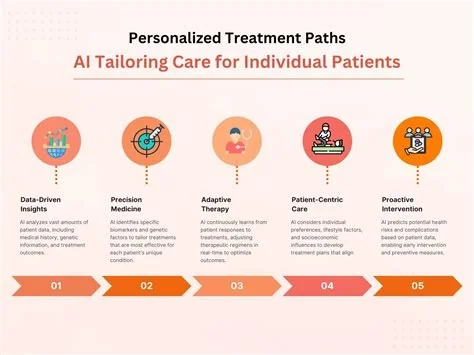
By incorporating contemporary treatment outcomes, the AI‑based model provides clinicians with a real‑time, evidence‑based tool to balance surgical benefits against potential morbidity. The system can be embedded in electronic health records, allowing surgeons and oncologists to generate individualized risk profiles during pre‑operative planning.
Future Validation and Integration
While initial results are promising, external validation on international datasets is planned to confirm the model’s generalizability across diverse health‑care settings. Successful validation could lead to routine use of the scoring system in multidisciplinary tumor boards, guiding decisions from aggressive resection to hospice‑focused care.
Next Steps
Ongoing collaborations aim to test the algorithm on larger, heterogeneous patient populations and to refine the user interface for seamless integration into clinical workflows.
Benefits for Patients and Providers
For patients, a more accurate survival estimate clarifies expectations and supports shared decision‑making. For providers, the model reduces reliance on outdated heuristics, enabling a data‑driven approach that aligns with the latest oncologic advances. As AI continues to permeate clinical practice, tools like this prognostic score translate large‑scale prospective data into actionable bedside insights.